Investigating Whether the Mediterranean Dietary Pattern Is Integrated in Routine Dietetic Practice for Management of Chronic Conditions: A National Survey of Dietitians
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Survey Development
2.3. Data Analysis
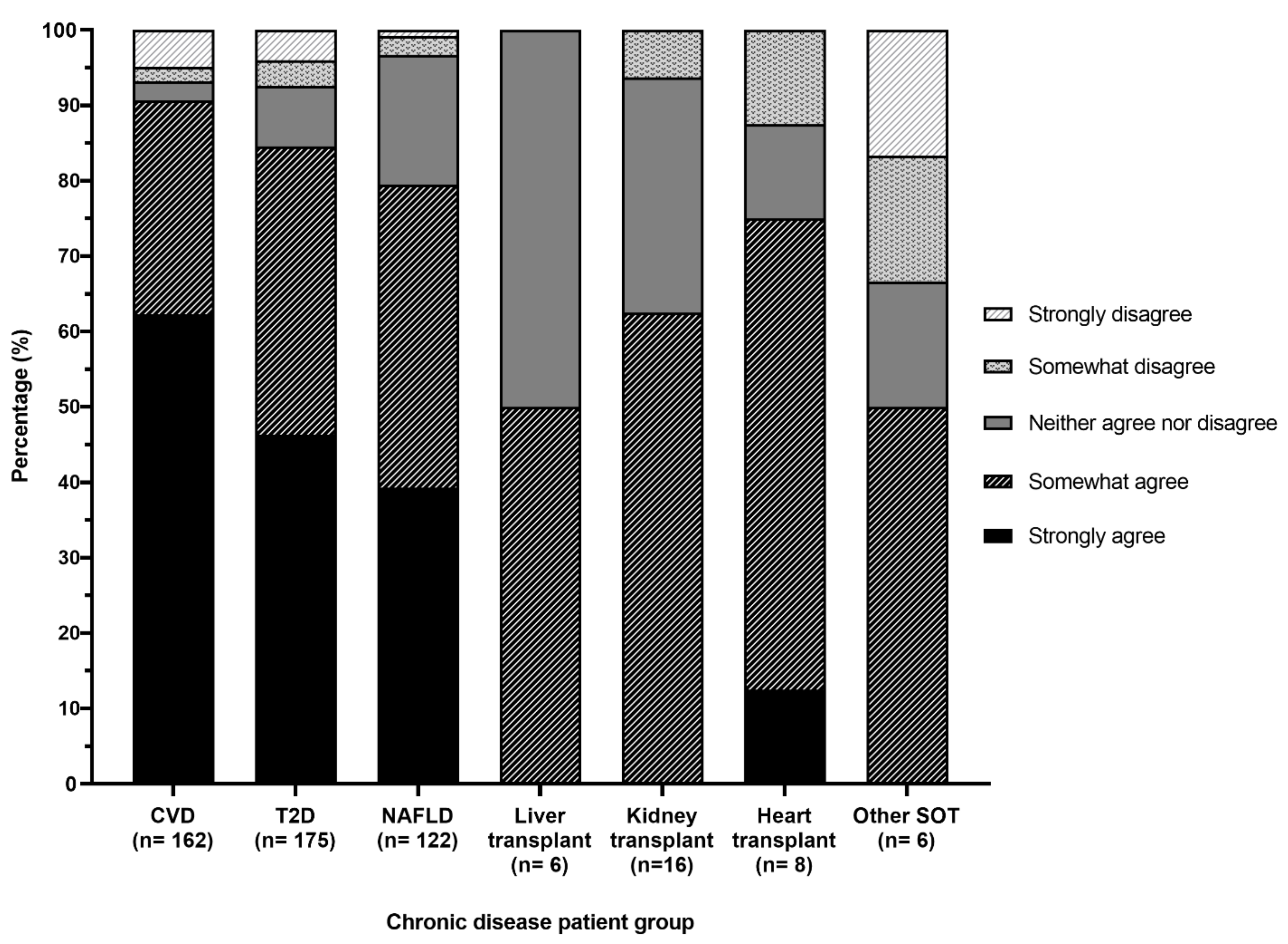
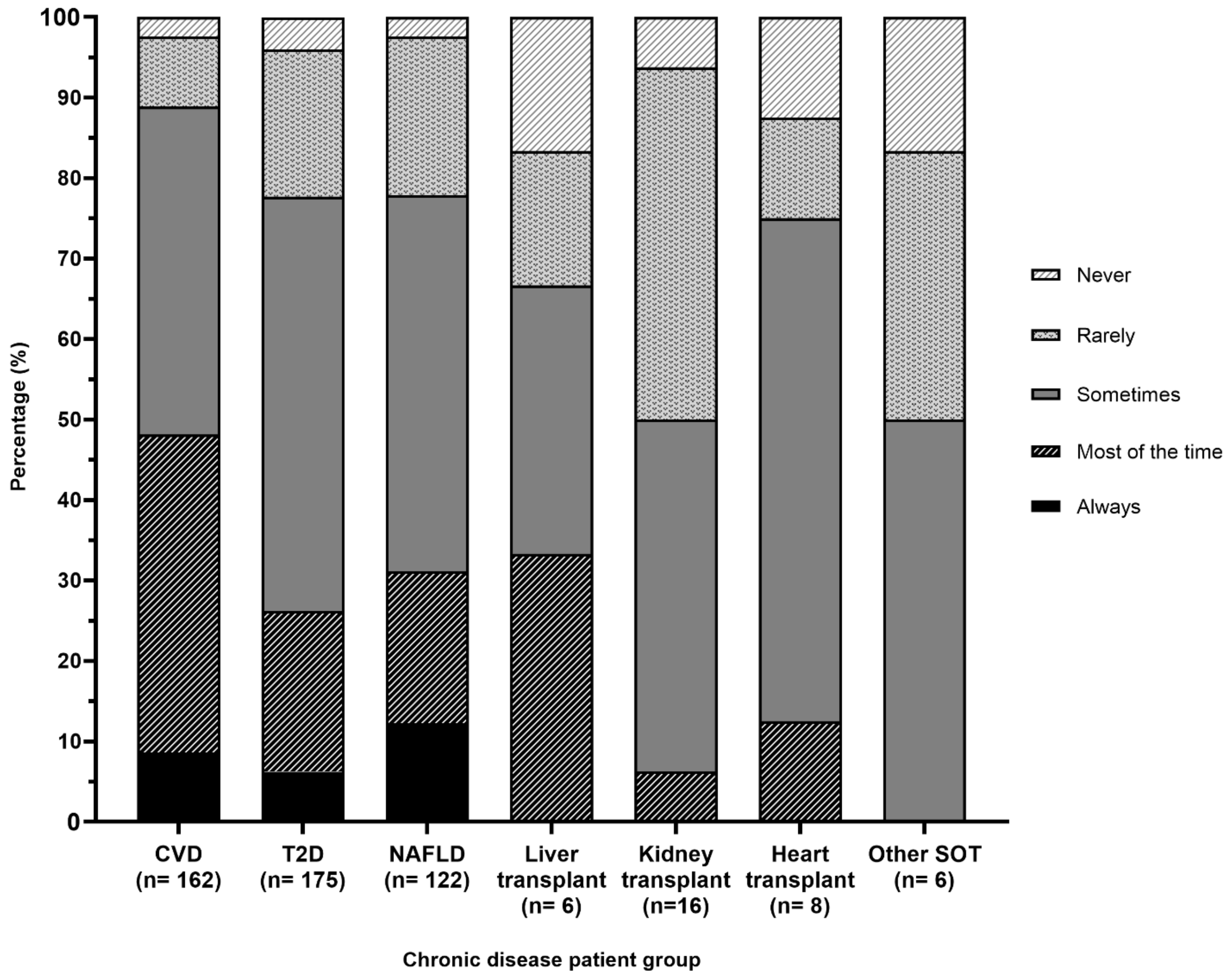
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Murray, C.J.L.; Vos, T.; Lozano, R.; Naghavi, M.; Flaxman, A.D.; Michaud, C.; Ezzati, M.; Shibuya, K.; Salomon, J.A.; Abdalla, S.; et al. Disability-adjusted life years (dalys) for 291 diseases and injuries in 21 regions, 1990–2010: A systematic analysis for the global burden of disease study 2010. Lancet 2012, 380, 2197–2223. [Google Scholar] [CrossRef]
- Targher, G.; Byrne, C.D. Nonalcoholic fatty liver disease: A novel cardiometabolic risk factor for type 2 diabetes and its complications. J. Clin. Endocrinol. Metab. 2013, 98, 483–495. [Google Scholar] [CrossRef]
- Wang, C.C.L.; Hess, C.N.; Hiatt, W.R.; Goldfine, A.B. Clinical update: Cardiovascular disease in diabetes mellitus. Circulation 2016, 133, 2459–2502. [Google Scholar] [CrossRef]
- Australian Institute of Health and Welfare. Risk Factors Contributing to Chronic Disease; Cat no. Phe 157; AIHW: Canberra, Australia, 2012.
- European Association for the Study of the Liver; European Association for the Study of Diabetes; European Association for the Study of Obesity. EASL-EASD-EASO clinical practice guidelines for the management of non-alcoholic fatty liver disease. Obes. Facts 2016, 9, 65–90. [Google Scholar] [CrossRef]
- American Diabetes Association. 5. Lifestyle management: Standards of medical care in diabetes 2019. Diabetes Care 2019, 42, S46–S60. [Google Scholar] [CrossRef] [PubMed]
- Amsterdam, E.A.; Wenger, N.K.; Brindis, R.G.; Casey, D.E., Jr.; Ganiats, T.G.; Holmes, D.R., Jr.; Jaffe, A.S.; Jneid, H.; Kelly, R.F.; Kontos, M.C.J.C. 2014 AHA/ACC guideline for the management of patients with non–st-elevation acute coronary syndromes: Executive summary: A report of the American college of cardiology/American heart association task force on practice guidelines. Circulation 2014, 130, 2354–2394. [Google Scholar] [CrossRef]
- Mozaffarian, D. Dietary and policy priorities for cardiovascular disease, diabetes, and obesity: A comprehensive review. Circulation 2016, 133, 187–225. [Google Scholar] [CrossRef]
- Willett, W.C.; Sacks, F.; Trichopoulou, A.; Drescher, G.; Ferro-Luzzi, A.; Helsing, E.; Trichopoulos, D. Mediterranean diet pyramid: A cultural model for healthy eating. Am. J. Clin. Nutr. 1995, 61, 1402S–1406S. [Google Scholar] [CrossRef]
- Bach-Faig, A.; Berry, E.M.; Lairon, D.; Reguant, J.; Trichopoulou, A.; Dernini, S.; Medina, F.X.; Battino, M.; Belahsen, R.; Miranda, G. Mediterranean diet pyramid today. Science and cultural updates. Public Health Nutr. 2011, 14, 2274–2284. [Google Scholar] [CrossRef]
- Davis, C.; Bryan, J.; Hodgson, J.; Murphy, K. Definition of the Mediterranean diet: A literature review. Nutrients 2015, 7, 9139–9153. [Google Scholar] [CrossRef]
- Dinu, M.; Pagliai, G.; Casini, A.; Sofi, F. Mediterranean diet and multiple health outcomes: An umbrella review of meta-analyses of observational studies and randomised trials. Eur. J. Clin. Nutr. 2018, 72, 30–43. [Google Scholar] [CrossRef] [PubMed]
- Schwingshackl, L.; Hoffmann, G. Mediterranean dietary pattern, inflammation and endothelial function: A systematic review and meta-analysis of intervention trials. Nutr. Metab. Cardiovasc. Dis. 2014, 24, 929–939. [Google Scholar] [CrossRef] [PubMed]
- Bendall, C.L.; Mayr, H.L.; Opie, R.S.; Bes-Rastrollo, M.; Itsiopoulos, C.; Thomas, C.J. Central obesity and the Mediterranean diet: A systematic review of intervention trials. Crit. Rev. Food Sci. Nutr. 2018, 58, 3070–3084. [Google Scholar] [CrossRef]
- Ryan, M.C.; Itsiopoulos, C.; Thodis, T.; Ward, G.; Trost, N.; Hofferberth, S.; O’Dea, K.; Desmond, P.V.; Johnson, N.A.; Wilson, A.M. The Mediterranean diet improves hepatic steatosis and insulin sensitivity in individuals with non-alcoholic fatty liver disease. J. Hepatol. 2013, 59, 138–143. [Google Scholar] [CrossRef]
- Serra-Majem, L.; Roman, B.; Estruch, R. Scientific evidence of interventions using the Mediterranean diet: A systematic review. Nutr. Rev. 2006, 64, S27–S47. [Google Scholar] [CrossRef]
- Davis, C.R.; Hodgson, J.M.; Woodman, R.; Bryan, J.; Wilson, C.; Murphy, K.J. A Mediterranean diet lowers blood pressure and improves endothelial function: Results from the MEDLEY randomized intervention trial. Am. J. Clin. Nutr. 2017, 105, 1305–1313. [Google Scholar] [CrossRef]
- Fox, C.S.; Golden, S.H.; Anderson, C.; Bray, G.A.; Burke, L.E.; De Boer, I.H.; Deedwania, P.; Eckel, R.H.; Ershow, A.G.; Fradkin, J. Update on prevention of cardiovascular disease in adults with type 2 diabetes mellitus in light of recent evidence: A scientific statement from the American heart association and the American diabetes association. Circulation 2015, 132, 691–718. [Google Scholar] [CrossRef]
- The Royal Australian College of General Practitioners. General Practice Management of Type 2 Diabetes: 2016–2018; RACGP: East Melbourne, Australia, 2016. [Google Scholar]
- Natrional Heart Foundation of Australia. Dietary Position Statement. Heart Healthy Eating Patterns; National Heart Foundation of Australia: Melbourne, Australia, 2019. [Google Scholar]
- Diabetes UK. Evidence-Based Nutrition Guidelines for the Prevention and Management of Diabetes; Diabetes UK: London, UK, 2018. [Google Scholar]
- Plauth, M.; Bernal, W.; Dasarathy, S.; Merli, M.; Plank, L.D.; Schütz, T.; Bischoff, S.C. ESPEN guideline on clinical nutrition in liver disease. Clin. Nutr. 2019, 38, 485–521. [Google Scholar] [CrossRef]
- Bamgbola, O. Metabolic consequences of modern immunosuppressive agents in solid organ transplantation. Ther. Adv. Endocrinol. Metab. 2016, 7, 110–127. [Google Scholar] [CrossRef]
- Munagala, M.R.; Phancao, A. Managing cardiovascular risk in the post solid organ transplant recipient. Med. Clin. 2016, 100, 519–533. [Google Scholar] [CrossRef]
- Morris, Z.S.; Wooding, S.; Grant, J. The answer is 17 years, what is the question: Understanding time lags in translational research. J. R. Soc. Med. 2011, 104, 510–520. [Google Scholar] [CrossRef]
- Martínez-González, M.Á.; Hershey, M.S.; Zazpe, I.; Trichopoulou, A. Transferability of the Mediterranean diet to non-Mediterranean countries. What is and what is not the Mediterranean diet. Nutrients 2017, 9, 1226. [Google Scholar] [CrossRef]
- Kuritzky, L.; Lang, S. The Mediterranean diet: Lost in translation. Curr. Hypertens. Rep. 2018, 20, 104. [Google Scholar] [CrossRef]
- Middleton, G.; Keegan, R.; Smith, M.F.; Alkhatib, A.; Klonizakis, M. Implementing a Mediterranean diet intervention into a RCT: Lessons learned from a non-Mediterranean based country. J. Nutr. Health Aging 2015, 19, 1019–1022. [Google Scholar] [CrossRef]
- Davis, C.; Hodgson, J.; Bryan, J.; Garg, M.; Woodman, R.; Murphy, K. Older australians can achieve high adherence to the Mediterranean diet during a 6 month randomised intervention; results from the MEDLEY study. Nutrients 2017, 9, 534. [Google Scholar] [CrossRef]
- Jacka, F.N.; O’Neil, A.; Opie, R.; Itsiopoulos, C.; Cotton, S.; Mohebbi, M.; Castle, D.; Dash, S.; Mihalopoulos, C.; Chatterton, M.L. A randomised controlled trial of dietary improvement for adults with major depression (the ‘SMILES’trial). BMC Med. 2017, 15, 23. [Google Scholar] [CrossRef] [PubMed]
- Itsiopoulos, C.; Brazionis, L.; Kaimakamis, M.; Cameron, M.; Best, J.D.; O’Dea, K.; Rowley, K. Can the Mediterranean diet lower hba1c in type 2 diabetes? Results from a randomized cross-over study. Nutr. Metab. Cardiovasc. Dis. 2011, 21, 740–747. [Google Scholar] [CrossRef]
- Mayr, H.L.; Itsiopoulos, C.; Tierney, A.C.; Ruiz-Canela, M.; Hebert, J.R.; Shivappa, N.; Thomas, C.J. Improvement in dietary inflammatory index score after 6-month dietary intervention is associated with reduction in interleukin-6 in patients with coronary heart disease: The AUSMED heart trial. Nutr. Res. 2018, 55, 108–121. [Google Scholar] [CrossRef] [PubMed]
- Properzi, C.; O’Sullivan, T.A.; Sherriff, J.L.; Ching, H.L.; Jeffrey, G.P.; Buckley, R.F.; Tibballs, J.; MacQuillan, G.C.; Garas, G.; Adams, L.A. Ad libitum Mediterranean and low-fat diets both significantly reduce hepatic steatosis: A randomized controlled trial. Hepatology 2018, 68, 1741–1754. [Google Scholar] [CrossRef]
- Australian Government Department of Health. Medicare Benefits Schedule—Item 10954. Available online: http://www9.health.gov.au/mbs/fullDisplay.cfm?type=item&q=10954&qt=item (accessed on 29 October 2020).
- Knights, S.; Tapsell, L. Dietetic practice in type 2 diabetes: An ethnographic study of Australian dietitians. Nutr. Diet. 2007, 64, 7–15. [Google Scholar] [CrossRef]
- McArdle, P.D.; Greenfield, S.M.; Avery, A.; Adams, G.G.; Gill, P.S. Dietitians’ practice in giving carbohydrate advice in the management of type 2 diabetes: A mixed methods study. J. Hum. Nutr. Diet. 2017, 30, 385–393. [Google Scholar] [CrossRef]
- Von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gøtzsche, P.C.; Vandenbroucke, J.P. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: Guidelines for reporting observational studies. Ann. Intern. Med. 2007, 147, 573–577. [Google Scholar] [CrossRef]
- Cane, J.; O’Connor, D.; Michie, S. Validation of the theoretical domains framework for use in behaviour change and implementation research. Implement. Sci. 2012, 7, 37. [Google Scholar] [CrossRef] [PubMed]
- George, E.S.; Kucianski, T.; Mayr, H.L.; Moschonis, G.; Tierney, A.C.; Itsiopoulos, C. A Mediterranean diet model in australia; strategies for translating the traditional Mediterranean diet into a multicultural setting. Nutrients 2018, 10, 465. [Google Scholar] [CrossRef]
- Estruch, R.; Ros, E.; Salas-Salvadó, J.; Covas, M.I.; Corella, D.; Arós, F.; Gómez-Gracia, E.; Ruiz-Gutiérrez, V.; Fiol, M.; Lapetra, J. Primary prevention of cardiovascular disease with a Mediterranean diet supplemented with extra-virgin olive oil or nuts. N. Engl. J. Med. 2018, 378, e34. [Google Scholar] [CrossRef]
- Health Workforce Australia. Australia’s Health Workforce Series. Dietitians in Focus; Health Workforce Australia: Adelaide, Australia, 2014.
- Dietitians Australia. Annual Report 2018–2019; Dietitians Australia: Canberra, Australia, 2019. [Google Scholar]
- Kouris-Blazos, A.; Gnardellis, C.; Wahlqvist, M.L.; Trichopoulos, D.; Lukito, W.; Trichopoulou, A. Are the advantages of the Mediterranean diet transferable to other populations? A cohort study in Melbourne, Australia. Br. J. Nutr. 1999, 82, 57–61. [Google Scholar] [CrossRef]
- Mantzioris, E.; Villani, A. Translation of a Mediterranean-style diet into the Australian dietary guidelines: A nutritional, ecological and environmental perspective. Nutrients 2019, 11, 2507. [Google Scholar] [CrossRef]
- Young, A.M.; Olenski, S.; Wilkinson, S.A.; Campbell, K.; Barnes, R.; Cameron, A.; Hickman, I. Knowledge translation in dietetics: A survey of dietitians’ awareness and confidence. Can. J. Diet. Pract. Res. 2019, 81, 49–53. [Google Scholar] [CrossRef]
- Soguel, L.; Vaucher, C.; Bengough, T.; Burnand, B.; Desroches, S. Knowledge translation and evidence-based practice: A qualitative study on clinical dietitians’ perceptions and practices in Switzerland. J. Acad. Nutr. Diet. 2019, 119, 1882–1889. [Google Scholar] [CrossRef]
- Byham-Gray, L.D.; Gilbride, J.A.; Dixon, L.B.; Stage, F.K. Evidence-based practice: What are dietitians’ perceptions, attitudes, and knowledge? J. Am. Diet. Assoc. 2005, 105, 1574–1581. [Google Scholar] [CrossRef]
- Hébert, J.R.; Frongillo, E.A.; Adams, S.A.; Turner-McGrievy, G.M.; Hurley, T.G.; Miller, D.R.; Ockene, I.S. Perspective: Randomized controlled trials are not a panacea for diet-related research. Adv. Nutr. 2016, 7, 423–432. [Google Scholar] [CrossRef]
- Milosavljevic, M.; Williams, P.; Perez, G.; Dalla, T. The results of a pilot time-and-motion study in three Australian hospitals: Where do we spend our time? Nutr. Diet. 2011, 68, 185–188. [Google Scholar] [CrossRef]
- Segal, L.; Opie, R.S. A nutrition strategy to reduce the burden of diet related disease: Access to dietician services must complement population health approaches. Front. Pharmacol. 2015, 6, 160. [Google Scholar] [CrossRef]
- Orazio, L.K.; Murray, E.M.; Campbell, K.L. Guideline use: A survey of dietitians working with adult kidney transplant recipients. Nephrology 2012, 17, 508–513. [Google Scholar] [CrossRef]
- Hickman, I.J.; Coran, D.; Wallen, M.P.; Kelly, J.; Barnett, A.; Gallegos, D.; Jarrett, M.; McCoy, S.M.; Campbell, K.L.; Macdonald, G.A. ‘Back to life’—Using knowledge exchange processes to enhance lifestyle interventions for liver transplant recipients: A qualitative study. Nutr. Diet. 2019, 76, 399–406. [Google Scholar] [CrossRef]
- Organ and Tissue Authority. 2019 Australian Donation and Transplantation Activity Report; Australian Government: Canberra, Australia, 2020.
- Patel, P.J.; Banh, X.; Horsfall, L.U.; Hayward, K.L.; Hossain, F.; Johnson, T.; Stuart, K.A.; Brown, N.N.; Saad, N.; Clouston, A.; et al. Underappreciation of non-alcoholic fatty liver disease by primary care clinicians: Limited awareness of surrogate markers of fibrosis. Intern. Med. J. 2018, 48, 144–151. [Google Scholar] [CrossRef] [PubMed]
- National Health and Medical Research Council. Australian Dietary Guidelines; NHMRC: Canberra, Australia, 2013.
- Mayr, H.L.; Thomas, C.J.; Tierney, A.C.; Kucianski, T.; George, E.S.; Ruiz-Canela, M.; Hebert, J.R.; Shivappa, N.; Itsiopoulos, C. Randomization to 6-month Mediterranean diet compared with a low-fat diet leads to improvement in dietary inflammatory index scores in patients with coronary heart disease: The AUSMED heart trial. Nutr. Res. 2018, 55, 94–107. [Google Scholar] [CrossRef]
- Urpi-Sarda, M.; Casas, R.; Chiva-Blanch, G.; Romero-Mamani, E.S.; Valderas-Martínez, P.; Arranz, S.; Andres-Lacueva, C.; Llorach, R.; Medina-Remón, A.; Lamuela-Raventos, R.M. Virgin olive oil and nuts as key foods of the Mediterranean diet effects on inflammatory biomarkers related to atherosclerosis. Pharmacol. Res. 2012, 65, 577–583. [Google Scholar] [CrossRef] [PubMed]
- de Alvarenga, J.F.R.; Tran, C.; Hurtado-Barroso, S.; Martinez-Huélamo, M.; Illan, M.; Lamuela-Raventos, R.M. Home cooking and ingredient synergism improve lycopene isomer production in sofrito. Food Res. Int. 2017, 99, 851–861. [Google Scholar] [CrossRef]
- Shivappa, N.; Steck, S.E.; Hurley, T.G.; Hussey, J.R.; Hébert, J.R. Designing and developing a literature-derived, population-based dietary inflammatory index. Public Health Nutr. 2014, 17, 1689–1696. [Google Scholar] [CrossRef]
- National Heart Foundation of Australia; Cardiac Society of Australia and New Zealand. Reducing Risk in Heart Disease: An Expert Guide to Clinical Practice for Secondary Prevention of Coronary Heart Disease; NHF; CSANZ: Melbourne, Australia, 2012. [Google Scholar]
- Haigh, L.; Bremner, S.; Houghton, D.; Henderson, E.; Avery, L.; Hardy, T.; Hallsworth, K.; McPherson, S.; Anstee, Q.M. Barriers and facilitators to Mediterranean diet adoption by patients with nonalcoholic fatty liver disease in northern europe. Clin. Gastroenterol. Hepatol. 2019, 17, 1364–1371.e1363. [Google Scholar] [CrossRef]
- Barnett, A.; Campbell, K.L.; Mayr, H.L.; Keating, S.E.; Macdonald, G.A.; Hickman, I.J. Liver transplant recipients’ experiences and perspectives of a telehealth-delivered lifestyle programme: A qualitative study. J. Telemed. Telecare 2020. [Google Scholar] [CrossRef]
- Moore, S.E.; McEvoy, C.T.; Prior, L.; Lawton, J.; Patterson, C.C.; Kee, F.; Cupples, M.; Young, I.S.; Appleton, K.; McKinley, M.C.; et al. Barriers to adopting a Mediterranean diet in Northern European adults at high risk of developing cardiovascular disease. J. Hum. Nutr. Diet. 2018, 31, 451–462. [Google Scholar] [CrossRef]
- Bonaccio, M.; Di Castelnuovo, A.; Costanzo, S.; De Lucia, F.; Olivieri, M.; Donati, M.B.; de Gaetano, G.; Iacoviello, L.; Bonanni, A. Mass media information and adherence to Mediterranean diet: Results from the Moli-sani study. Int. J. Public Health 2012, 57, 589–597. [Google Scholar] [CrossRef]
- Siopis, G.; Jones, A.; Allman-Farinelli, M. The dietetic workforce distribution geographic atlas provides insight into the inequitable access for dietetic services for people with type 2 diabetes in Australia. Nutr. Diet. 2020, 77, 121–130. [Google Scholar] [CrossRef]
- Australian Institute of Health and Welfare. Australia’s Health 2018. Australia’s Health Series no. 16 aus 221; AIHW: Canberra, Australia, 2018.
- Opie, R.S.; Segal, L.; Jacka, F.N.; Nicholls, L.; Dash, S.; Pizzinga, J.; Itsiopoulos, C. Assessing healthy diet affordability in a cohort with major depressive disorders. JPHE 2015, 7, 159–169. [Google Scholar]
- Goulet, J.; Lamarche, B.; Lemieux, S. A nutritional intervention promoting a Mediterranean food pattern does not affect total daily dietary cost in North American women in free-living conditions. J. Nutr. 2008, 138, 54–59. [Google Scholar] [CrossRef]
- Papadaki, A.; Scott, J.A. Process evaluation of an innovative healthy eating website promoting the Mediterranean diet. Health Educ. Res. 2005, 21, 206–218. [Google Scholar] [CrossRef] [PubMed]
- Itsiopoulos, C. The Mediterranean Diet; Pan MacMillan Australia: Sydney, Australia, 2013. [Google Scholar]
- Queensland Health Nutrition Education Materials Online. The Mediterranean Diet; Queensland Government: Brisbane, Australia, 2019.
- Peterson, L.; Carlos, D. Two Greek Girls Cooking. Available online: https://twogreekgirls.com/cook-book/ (accessed on 9 August 2020).
- Opie, R.S.; O’Neil, A.; Jacka, F.N.; Pizzinga, J.; Itsiopoulos, C. A modified Mediterranean dietary intervention for adults with major depression: Dietary protocol and feasibility data from the SMILES trial. Nutr. Neurosci. 2017, 21, 487–501. [Google Scholar] [CrossRef]
- Oldways. Traditional Diets. Mediterranean Diet. Available online: https://oldwayspt.org/traditional-diets/mediterranean-diet (accessed on 9 August 2020).
- Dietitians of Canada. Mediterranean Diet Toolkit: Supporting Patients to Reduce CVD Risk and Improve Mental Health; Dietitians of Canada: Toronto, ON, Canada, 2018. [Google Scholar]
- Kelly, J.T.; Reidlinger, D.P.; Hoffmann, T.C.; Campbell, K.L. Telehealth methods to deliver dietary interventions in adults with chronic disease: A systematic review and meta-analysis, 2. Am. J. Clin. Nutr. 2016, 104, 1693–1702. [Google Scholar] [CrossRef]
- Ball, L.; Ball, D.; Leveritt, M.; Ray, S.; Collins, C.; Patterson, E.; Ambrosini, G.; Lee, P.; Chaboyer, W. Using logic models to enhance the methodological quality of primary health-care interventions: Guidance from an intervention to promote nutrition care by general practitioners and practice nurses. Aust. J. Prim. Health 2017, 23, 53–60. [Google Scholar] [CrossRef]
| Characteristics | N (%) |
|---|---|
| Gender (female) | 177 (97) |
| Age (years), median (IQR) | 34 (29–44) |
| Born in Australia | 146 (81) |
| Mediterranean background a | 11 (6) |
| Time since graduating as a dietitian (years), median (IQR) (n = 180) | 9 (4–18) |
| <1 | 10 (6) |
| 1–5 | 50 (28) |
| 6–10 | 44 (24) |
| 11–15 | 23 (13) |
| 16–20 | 20 (11) |
| 20+ | 33 (18) |
| Duration practicing with relevant chronic conditions (years) | |
| <1 | 9 (5) |
| 1–5 | 64 (35) |
| 6–10 | 47 (26) |
| 11–15 | 24 (13) |
| 16–20 | 14 (8) |
| 20+ | 24 (13) |
| Main work location | |
| Metropolitan | 120 (66) |
| Regional | 39 (21) |
| Rural | 23 (13) |
| Main place of work | |
| Public Hospital | 68 (37) |
| Private Hospital | 6 (3) |
| Public Community Health Service | 39 (21) |
| Private Community Practice | 62 (34) |
| Aged Care | 2 (1) |
| Corporate Health | 2 (1) |
| Non-Government Organisation | 3 (2) |
| Main patient setting | |
| Acute | 36 (20) |
| Sub-acute | 10 (6) |
| Outpatient | 70 (39) |
| Community | 66 (36) |
| Prior education, training or self-study on MDP (n = 178) | 110 (62) |
| Dietetics degree b | 53 (30) |
| Professional development provided at work | 21 (12) |
| Professional development accessed outside of work (not a conference) | 71 (40) |
| Reading scientific literature | 83 (47) |
| Australian conference | 37 (21) |
| International conference | 2 (1) |
| Research activities | 20 (11) |
| Other | 8 (4) |
| Question | Strongly Disagree | Somewhat Disagree | Neither Agree Nor Disagree | Somewhat Agree | Strongly Agree |
|---|---|---|---|---|---|
| N (%) | |||||
| I am knowledgeable of the principles of the MDP | 3 (2) | 1 (1) | 5 (3) | 86 (47) | 87 (48) |
| I am confident to describe to a colleague the key principles of the MDP | 2 (1) | 5 (3) | 5 (3) | 83 (46) | 87 (48) |
| I am confident to counsel a patient to follow the principles of the MDP | 2 (1) | 7 (4) | 11 (6) | 78 (43) | 83 (46) |
| Recommending the MDP to patients with chronic disease is part of my role | 4 (2) | 11 (6) | 32 (18) | 82 (45) | 53 (29) |
| MDP Principle a | Never | Rarely | Sometimes | Most of the Time | Always |
|---|---|---|---|---|---|
| N (%) | |||||
| Daily intake of fruit (2–3 serves) | 1 (1) | 3 (2) | 19 (11) | 53 (30) | 102 (58) |
| Daily intake of vegetables (5 or more serves) | 1 (1) | 2 (1) | 10 (6) | 36 (20) | 129 (73) |
| Daily intake of tomatoes | 43 (24) | 52 (29) | 55 (31) | 22 (12) | 6 (3) |
| Daily intake of leafy green salads/vegetables | 9 (5) | 12 (7) | 37 (21) | 56 (32) | 64 (36) |
| Regular use of onion and garlic in cooking | 30 (17) | 45 (25) | 63 (35) | 32 (18) | 8 (5) |
| Regular use of herbs and spices in cooking | 10 (6) | 21 (12) | 63 (35) | 57 (32) | 27 (15) |
| Daily intake of wholegrain cereals (6–8 serves) | 3 (2) | 10 (6) | 37 (21) | 72 (40) | 56 (32) |
| Use of extra virgin olive oil as the main dietary fat | 1 (0.6) | 6 (3) | 37 (21) | 52 (29) | 82 (46) |
| Daily intake of extra virgin olive oil 3–4 tablespoons per day | 33 (19) | 47 (26) | 56 (32) | 28 (16) | 14 (8) |
| Intake of fermented dairy foods (yoghurt and cheese) on most days | 12 (7) | 21 (12) | 51 (29) | 60 (34) | 34 (19) |
| Limit intake of red meat to no more than 1 serve per week | 18 (10) | 49 (28) | 56 (32) | 46 (26) | 9 (5) |
| Limit intake of processed/deli meats and small goods | 1 (1) | 4 (2) | 10 (6) | 64 (36) | 99 (56) |
| Regular intake of legumes/lentils (2 or more serves per week) | 0 | 17 (10) | 50 (28) | 59 (33) | 52 (29) |
| Regular intake of fish/seafood (3 or more serves per week) b (n = 95) | 0 | 2 (2) | 16 (17) | 44 (46) | 33 (35) |
| Intake of nuts on most days | 1 (1) | 14 (8) | 51 (29) | 64 (27) | 48 (27) |
| If choosing to drink alcohol, moderate consumption of wine (1–2 glasses per day) with meals | 7 (4) | 25 (14) | 38 (21) | 60 (34) | 48 (27) |
| Limit intake of sugary drinks | 0 | 1 (1) | 7 (4) | 31 (17) | 139 (78) |
| Limit intake of commercial or processed sweets/goods/savoury snacks | 2 (1) | 0 | 6 (3) | 46 (26) | 124 (70) |
| Encourage eating with others or shared meals | 5 (3) | 22 (12) | 59 (33) | 47 (26) | 45 (25) |
| Encourage home cooking | 1 (1) | 1 (1) | 19 (11) | 79 (44) | 78 (44) |
| Increasing regular physical activity (n = 170) | 1 (1) | 6 (4) | 46 (27) | 67 (39) | 50 (29 |
| Would you estimate that you personally follow a MDP? | 2 (1) | 4 (2) | 66 (37) | 91 (51) | 15 (8) |
| How often do other dietitians that you work with or know recommend the MDP to patients with chronic disease? N = 81 (45%) responded ‘I don’t know’ | 2 (1) | 8 (4) | 62 (34) | 24 (13) | 5 (3) |
| Question | More Often a Barrier | More Often an Enabler | Both a Barrier and an Enabler | Neither a Barrier or an Enabler | Not Relevant to My Practice |
|---|---|---|---|---|---|
| N (%) | |||||
| Access to or awareness of relevant evidence/practice guidelines | 22 (13) | 82 (48) | 24 (14) | 42 (25) | 1 (1) |
| Access to or awareness of professional development, education or training for dietitians | 36 (21) | 77 (45) | 23 (14) | 33 (19) | 2 (1) |
| Access to or awareness of relevant patient education materials or resources | 52 (30) | 69 (40) | 20 (12) | 28 (16) | 2 (1) |
| Acceptability of the diet principles by patients | 38 (22) | 56 (33) | 54 (32) | 21 (12) | 2 (1) |
| Goals or motivation of patients in relation to diet | 44 (26) | 49 (29) | 58 (34) | 19 (11) | 1 (1) |
| Your own cultural background | 7 (4) | 53 (31) | 15 (9) | 82 (48) | 14 (8) |
| Cultural background of your patient | 47 (28) | 21 (12) | 74 (43) | 27 (16) | 2 (1) |
| Support from/goals of the multi-disciplinary team or other clinicians treating your patient | 17 (10) | 45 (26) | 38 (22) | 56 (33) | 15 (9) |
| Reason for dietitian referral | 19 (11) | 49 (29) | 40 (23) | 56 (33) | 7 (4) |
| Time allocated to patient consultations | 65 (38) | 25 (15) | 15 (9) | 60 (35) | 6 (4) |
| Number of patient visits | 75 (44) | 24 (14) | 15 (9) | 50 (28) | 7 (4) |
| Cost of the diet | 49 (29) | 19 (11) | 40 (23) | 59 (35) | 4 (2) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mayr, H.L.; Kostjasyn, S.P.; Campbell, K.L.; Palmer, M.; Hickman, I.J. Investigating Whether the Mediterranean Dietary Pattern Is Integrated in Routine Dietetic Practice for Management of Chronic Conditions: A National Survey of Dietitians. Nutrients 2020, 12, 3395. https://doi.org/10.3390/nu12113395
Mayr HL, Kostjasyn SP, Campbell KL, Palmer M, Hickman IJ. Investigating Whether the Mediterranean Dietary Pattern Is Integrated in Routine Dietetic Practice for Management of Chronic Conditions: A National Survey of Dietitians. Nutrients. 2020; 12(11):3395. https://doi.org/10.3390/nu12113395
Chicago/Turabian StyleMayr, Hannah L., Sarah P. Kostjasyn, Katrina L. Campbell, Michelle Palmer, and Ingrid J. Hickman. 2020. "Investigating Whether the Mediterranean Dietary Pattern Is Integrated in Routine Dietetic Practice for Management of Chronic Conditions: A National Survey of Dietitians" Nutrients 12, no. 11: 3395. https://doi.org/10.3390/nu12113395
APA StyleMayr, H. L., Kostjasyn, S. P., Campbell, K. L., Palmer, M., & Hickman, I. J. (2020). Investigating Whether the Mediterranean Dietary Pattern Is Integrated in Routine Dietetic Practice for Management of Chronic Conditions: A National Survey of Dietitians. Nutrients, 12(11), 3395. https://doi.org/10.3390/nu12113395






